Last week I got a wonderful compliment from a badminton player who found my YouTube video on self-massage and the IT band. We are coming into the time of year where activity levels begin to spike for athletes and sure enough there will be the complement of IT band pain. However, there is a lot of varied information on the internet about how to work with it. So I’m compiling information I’ve gathered from some good sources as well as 13 years of clinical experience on what I feel are very effective, safe methods to alleviate IT band pain and discomfort.
It’s not a muscle!
Understanding the iliotibial band (IT band) and its purpose and function are critical in addressing any dysfunction associated with this structure that spans the distance from the hip to the knee. First and foremost it is important to understand that it is comprised of thick, dense connective tissue providing stability for the hip and lateral (outside) part of the knee. It is not a muscle; therefore it does not shorten and cannot be stretched or lengthened. It is really, really strong and durable because it has an important job to do maintaining stability for the hip and knee. I liken it to rebar, so keep that in mind when you attempt to “stretch” it or heaven forbid, use the foam roller on it (more on that later).
The IT band has vertical fibers that run along the lateral thigh. It begins up at the gluteal fascia, spans over the greater trochanter (bony outside part) of the hip, widens across and over top of the vastus lateralis (one of the four quadriceps femoris muscles) and then becomes very cable like as it attaches into the tibial tubercle (lateral aspect of the knee/tibia). Here is an excellent three minute video that shows you where the IT band and the tensor fasciae latae muscle are located.
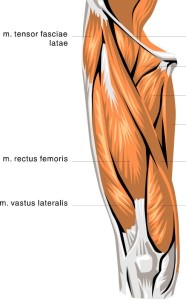
The IT band is the thin white band on the left side extending from tensor fasciae latae to the knee.
Why does it hurt so much?
So, just what in fact, does cause IT band pain? It seems to affect runners the most, as well as hikers, cyclists and obviously badminton players as stated earlier in this post. Thus it reasons to say that it probably affects players of other racquet sports as well. I know from personal experience that climbing upwards of five thousand or more vertical feet on a bike ride has caused my tensor fasciae latae muscle (TFL) to become very tired. Also, many of us have seen runners standing and hitting the TFL (located on the outside of the hip) with a soft fist after long runs. (Remember this, you’ll read more about TFL and its relationship to the IT band a little further on)
Whitney Lowe, from who I’ve taken continuing education classes, wrote in his book Orthopedic Assessment in Massage Therapy, “The ITB is under its greatest tension during the first third of the stance phase in running or walking. There is increased tension on the ITB when decelerating the body’s momentum, such as walking or running downhill.”
This makes sense to me, especially with greater awareness and education around proper running form. If a runner overstrides, with the foot striking well in front of the hip then the heel and leg have to act as somewhat of a braking mechanism before the runner rolls forward toward mid-foot and then accelerates off the ball of the foot. This repeated action, if a recreational runner has a cadence of say, 130 steps per minute (65 per foot) translates to 2600 hammering strikes to the IT band over the course of a 40 minute run! Conversely, elite runners have cadences as high as 180 rpm’s but have a much quicker, lighter turnover which helps to reduce injuries. The same could then be said that a hiker coming downhill on a steep trail should emphasize shorter steps in order to put less force into the ankles, knees and hips, thus reducing aggravation of the IT band.
The most obvious cause of any athletic overuse injury is an exercise program or activity that increases in volume or intensity too quickly. A common rule of thumb for increasing volume is 10% per week. While this may seem frustratingly slow, it is sound advice for forming a good foundation and avoiding injury while building a base of fitness.
It can be hard to describe the actual pain
Now I must mention here that in saying “IT band pain” we are speaking in somewhat vague terms. There is a specific condition called IT Band Friction Syndrome, which pertains to pain on the lateral part of the knee. This is pinpoint pain caused by the IT band passing over the distal part of the femur on the lateral aspect of the knee as the knee flexes and extends in the process of walking, running, cycling, etc. And this brings us to the problem of using a foam roller in a shotgun approach to IT band pain. Using a foam roller can be excruciatingly painful and because of continued misinformation people often think that attacking the IT Band with the foam roller will help resolve their issue; and sometimes it does help, but quite often it is in spite of this not because of it.
Knowing that the IT band is very dense, connective tissue and does not have the ability to shorten or contract let’s look at some structures that do in fact contract or shorten; muscles! There are two muscles that have a direct biomechanical impact on the IT band and others that I have found which can also be a contributing factor to IT band pain.
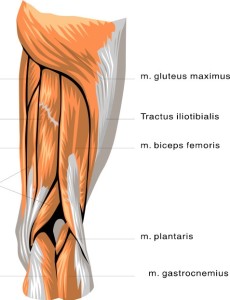
- Gluteus Maximus (yes, your butt!) – The lowest fibers of the gluteus maximus, the largest of the hip muscles, attaches to the IT band.
- Tensor Fasciae Latae (TFL) is a very short superficial muscle approximately three fingers wide that also attaches to the IT Band but a bit higher up than the gluteus maximus.
These two muscles can become tight enough where they can even exert force upon the IT band and thus begin to cause great discomfort and pain. In fact, in Whitney Lowe’s book, he writes “Excess tension in the ITB is a primary cause of ITB friction syndrome. The ITB is not a contractile tissue and tension differs from that of muscles. Excess tension in the ITB is due to hypertonicity of the tensor fasciae latae and gluteus maximus muscles that pull on the band.” (Emphasis is not added here, this is exactly how Whitney states it)
Be your own massage therapist!
Another muscle that I have found to contribute to IT band pain is vastus lateralis. This big quadricep femoris muscle runs underneath the IT band. This is where I have found adhesions on me and on many, many clients that occur between the vastus lateralis and the IT band, primarily on the bottom border of the IT band more frequently that on the top border. I think this is what people are trying to address when they begin steamrolling with the foam roller. But the foam roller ends up being a very general approach to the problem, instead of a targeted, specific approach. That is why people get varied results with the foam roller and other massage props or tools. The best tools are your hands and you’ll have a far greater chance of finding relief and actually feeling where the problem area is located. But keep that foam roller handy because it is a great tool for working the big gluteus maximus and also tensor fasciae latae. See, I’m not averse to the foam roller; I have one that I use numerous times per week on my own body, but I want to be sure to use the best tool for the job. So I’ll use a foam roller on my glutes, an elbow or the foam roller on my TFL and my fingertips and the mechanical force of rotating my hip to release the adhesions between my vastus lateralis and IT band. Check out my video on YouTube to see these very effective techniques that will help with prevention and alleviation of IT band pain.
Now, don’t be your own massage therapist!
Additionally, trigger points can cause referred pain into the IT band. And if that is the case, you can attack the IT band all you want but it won’t change the fact that the trigger points need to be resolved. Muscles that can have trigger point involvement with referral into the IT band might involve one or more of the following; tensor fasciae latae, vastus lateralis and especially gluteus minimus, which is a deep muscle in the hip. When it comes to trigger points I advise a person to seek out a qualified massage therapist or physiotherapist that has experience working with trigger points. In my massage practice I’ll warm the tissue, treat the trigger point with digital pressure and then quite often follow that up with specific stretches to resolve the trigger points. Many physiotherapists are now using dry needling in treating trigger points. The research is still pretty limited in the efficacy of treating trigger points with dry needling but this isn’t too far off the mark of the late Dr. Janet Travell, who I feel was and still is the authority on all things trigger points. Dr. Travell often used saline injections and vapocoolant spray in treating trigger points. Thus the current physios using dry needling haven’t reinvented the wheel but they treat the trigger points in a slightly different fashion than what Dr. Travell was doing.
What about stretching?
That brings us to stretching as a self-treatment tool. Here we move into the dark, murky waters of the efficiency of stretching. I’m not going to spend a lot of time on stretching but will highlight some important points on the matter.
- I advocate dynamic stretching and hands on self-massage to literally warm the muscle tissue and tendons before aerobic activity.
- I don’t favor static stretching (holding a stretch for 20-30 seconds) before heading out for activities such as running, cycling, soccer or any activity that involves quick, explosive movement and puts a heavy load on tendons and ligaments. It is possible to find research to support nearly any argument either for or against stretching. But I have moved more toward PNF (contract/relax) stretching, active or dynamic stretching in lieu of static stretching.
- I also highly recommend to my clients to actually stop moving and try self-massage if they are beginning to experience any niggling pain when exercising. If they are able to resume activity with no discomfort or it feels much better, then they have gained valuable information about what is contributing to their pain problem and can also communicate that back to me when I am treating them.
- After exercise or training is an appropriate time to stretch. I prefer movement incorporated active stretching such as the Active Isolated Stretching method by Aaron Mattes. Yoga postures are good as well. I’m a firm believer in exploring where you feel restriction or tightness versus a set stretching routine.
After proofing this I realized readers might be wondering about effective stretches for the IT band. Well, it is not a muscle so you won’t have much success with stretching it. You might want to give a stretch to TFL but it can be somewhat challenging to get a good stretch to it without assistance. Self-massage and foam rolling are your best bet and will lead to better function which will take tension off the IT band. This will likely help a lot more than trying to get a stretch into any of these areas.
Hopefully you’ll gain a better understanding of the IT band and the purpose of this post is to give you a sound knowledge of the IT band, its function and why it can be so mysterious in determining why pain is associated with it. The body is a very complex kinetic system so unfortunately there is no “magic pill” that will take care of your problems. The techniques that I describe above are techniques that I have found a lot of success with in treating IT band dysfunction, and with which my clients have been successful. However, each body is different and if pain lingers for any length of time then I highly recommend seeing a physical therapist or clinical massage therapist for a complete evaluation and assessment. Keep in mind that you are probably not a medical doctor so don’t pretend to be one by self-diagnosing on the internet! If you are apt to peruse the internet regarding conditions and good articles I recommend using schoIar.google.com. You will find only research based literature on that site. I welcome any comments or suggestions that you would like to see addressed!
Keep it safe, healthy and above all, have some FUN!

I am having problems with a very tight it band and glute on my left side. Was wondering your thoughts on B12 saline injections. I was told it would release the it band. Also wondering if it would revolve this issue.
Hi Judy,
The B12 saline injections fall outside of my scope of practice so I can’t offer any personal experience with them. I would confer with a physiotherapist or medical doctor about the efficacy of the treatment.
Best wishes for some healing and that you feel better.
Matt